Tooth extraction often sounds intimidating, but at Gurgaon Dental Hub, patients are experiencing a new level of comfort. With expert care at Dr. Futela's Dental Clinic, a trusted name in dental Gurgaon, extractions are now painless, stress-free, and performed in a calm, high-tech environment.
Whether you're dealing with a decayed tooth, wisdom tooth problems, or overcrowding, choosing the best dental clinic in Gurgaon ensures a smooth and comfortable experience. This post will explore everything you need to know about tooth extractions, what makes a dental clinic stand out, and why Dr. Futela's Dental Clinic is the top destination for dental care in Gurgaon.
Understanding Tooth Extraction: Why Is It Necessary?
Tooth extraction is the removal of a tooth from its socket in the bone. Although dentists always aim to save your natural teeth, there are situations where extraction becomes essential:
Severe Tooth Decay or Damage: When a tooth is beyond repair due to infection or trauma.
Impacted Wisdom Teeth: Often stuck in the gums, causing pain or risk of infection.
Orthodontic Treatment: Sometimes necessary to create space for proper alignment.
Gum Disease: Advanced periodontitis can loosen teeth, making extraction a solution.
Modern dentistry, especially at leading dental clinics in Gurgaon, uses advanced tools and sedation techniques to make this process safe and virtually painless.
The Myth of Painful Extractions: Breaking the Fear
Many patients associate dental treatments with discomfort, largely due to outdated tools or past experiences. But today, at top-rated clinics like Dr. Futela's Dental Clinic, tooth extractions are performed using cutting-edge methods and gentle care.
Digital X-rays for precise diagnosis
Local anesthesia to completely numb the area
Laser-assisted treatments for quicker healing
Conscious sedation options for anxious patients
Choosing the right clinic is key to overcoming dental anxiety. That’s why thousands trust Dr. Futela's Dental Clinic, a beacon for painless dental care in Gurgaon.
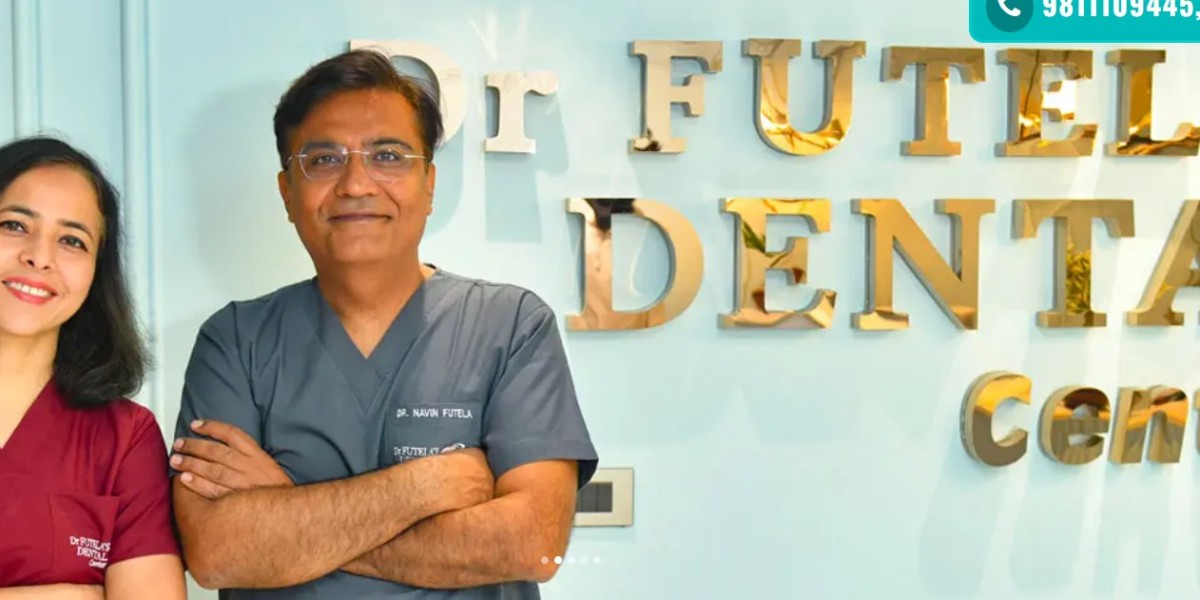
Meet Dr. Futela’s Dental Clinic: Best Dental Clinic in Gurgaon
Located in the heart of the city, Dr. Futela’s Dental Clinic is widely regarded as the best dental clinic in Gurgaon. With a team of highly experienced dentists, advanced infrastructure, and a patient-first approach, this clinic delivers world-class services.
What Makes Dr. Futela’s Stand Out?
Experienced Team: Led by Dr. Rahul Futela, with 15+ years in practice.
State-of-the-art Facilities: Digital X-rays, intraoral scanners, and pain-free extraction tools.
Personalized Care: Each patient receives a treatment plan tailored to their unique needs.
Sterilization Protocols: Highest standards of hygiene and safety.
Post-treatment Support: From aftercare guidance to recovery follow-ups, everything is managed meticulously.
Whether it’s a routine tooth removal or a complex surgical extraction, patients receive premium care with zero compromise on comfort.
How Painless Tooth Extraction Works at Dr. Futela’s Dental Clinic
Let’s walk through the step-by-step experience of getting a tooth extraction at this top dental Gurgaon clinic.
Step 1: Consultation & Diagnosis
Your journey starts with a thorough examination. Using digital X-rays and clinical evaluation, the dentist assesses the condition and decides if extraction is needed. At Dr. Futela’s, every step is explained to the patient.
Step 2: Pre-Procedure Preparation
On the day of the procedure:
You are seated in a relaxed environment.
Local anesthesia is administered to numb the area.
Sedation options like nitrous oxide are available for nervous patients.
Step 3: The Extraction Process
For simple extractions, the tooth is loosened and removed using special dental instruments.
For surgical extractions, a small incision may be made in the gum.
Thanks to modern equipment and expert hands, the entire process is quick, usually lasting only 15–30 minutes.
Step 4: Post-Extraction Care
After the tooth is removed, the dentist provides:
Gauze placement to control bleeding
Pain management and medication
Do’s and don’ts to aid faster healing
Recovery is typically smooth, especially when instructions are followed. Many patients return to normal activities within 24–48 hours.
Benefits of Choosing the Best Dental Clinic in Gurgaon
When it comes to oral health, don’t settle for less. Selecting the best dental clinic in Gurgaon, like Dr. Futela’s Dental Clinic, provides unmatched advantages:
1. Minimal Pain and Discomfort
The latest techniques minimize trauma, ensuring a painless experience. Patient testimonials frequently praise the “zero-pain” extractions at Dr. Futela’s.
2. Faster Recovery Time
Because of precision-based procedures, the surrounding tissues remain unaffected, reducing swelling and speeding up healing.
3. Comprehensive Aftercare
The clinic offers complete after-extraction support, including dietary advice, oral hygiene tips, and emergency contact access.
4. Expertise in Complicated Cases
For impacted or partially erupted teeth, expert surgical extraction is vital. Dr. Futela’s team is trained in handling such cases with ease.
5. Patient-Centric Atmosphere
From the front desk to the dental chair, every interaction is marked by empathy, professionalism, and genuine care.
What Patients Say About Tooth Extraction at Dr. Futela’s
“I was scared about getting my wisdom tooth out, but the team made it feel like a breeze. No pain, no fear. Highly recommend this dental Gurgaon clinic!” – Ananya S.
“I came in with a lot of anxiety. Dr. Futela took the time to explain everything and made me feel at ease. The extraction was quick and totally painless.” – Rajeev M.
Tips to Prepare for a Tooth Extraction
To ensure your experience is smooth, follow these tips before visiting the clinic:
Share full medical history with the dentist.
Avoid eating for a few hours if sedation is planned.
Arrange someone to accompany you if you’re nervous or sedated.
Follow pre-operative instructions given by the clinic.
Remember, your preparation plays a key role in a seamless extraction and recovery.
Post-Extraction Care: What to Expect
Healing is usually uncomplicated, especially when following these aftercare steps:
Avoid spitting or using straws for the first 24 hours.
Apply ice packs to reduce swelling.
Take prescribed medication exactly as advised.
Eat soft foods and avoid smoking or alcohol.
Brush gently, avoiding the extraction site.
If you face prolonged pain or signs of infection, contact the clinic immediately. At Dr. Futela’s Dental Clinic, patient safety is always the top priority.
Why Dental Care in Gurgaon Is Evolving Rapidly
The rise in demand for high-quality dental services in Gurgaon has encouraged clinics to upgrade their facilities and bring in global best practices. Today, dental Gurgaon clinics are equipped to deliver international-standard treatments at competitive prices.
With urban lifestyles increasing oral health issues like cavities, wisdom tooth problems, and gum diseases, patients seek:
Advanced diagnostics
Shorter recovery periods
Affordable yet premium treatment
Clinics like Dr. Futela’s have risen to meet these expectations, making Gurgaon a hub for modern dental care.
Final Thoughts: Book Your Painless Tooth Extraction Today
Tooth extraction no longer has to be a dreaded procedure. At Dr. Futela’s Dental Clinic, patients are treated to a world-class experience that prioritizes comfort, safety, and successful outcomes.
Choosing the best dental clinic in Gurgaon ensures that you’re in safe hands—from consultation to recovery. So if you’re experiencing tooth pain or have been advised an extraction, don’t wait. Visit Dr. Futela’s Dental Clinic—your trusted partner for painless dental care in Gurgaon.