Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) characterized by inflammation of the colon and rectum, leading to debilitating symptoms and affecting quality of life. This Ulcerative Colitis Epidemiology Analysis provides insights into prevalence, risk factors, and the global burden of the disease, highlighting the need for improved awareness, research, and therapeutic strategies.
Introduction to Ulcerative Colitis Epidemiology
Ulcerative colitis, often diagnosed in early adulthood, is a lifelong condition requiring ongoing management. The disease's epidemiology varies significantly across regions, influenced by genetic, environmental, and lifestyle factors. With rising incidence rates in emerging economies, UC is becoming a pressing global health concern.
Understanding UC's epidemiology is crucial for tailoring healthcare resources, advancing treatments, and improving patient outcomes.
Global Prevalence and Incidence of Ulcerative Colitis
What is Epidemiology in the Context of Ulcerative Colitis?
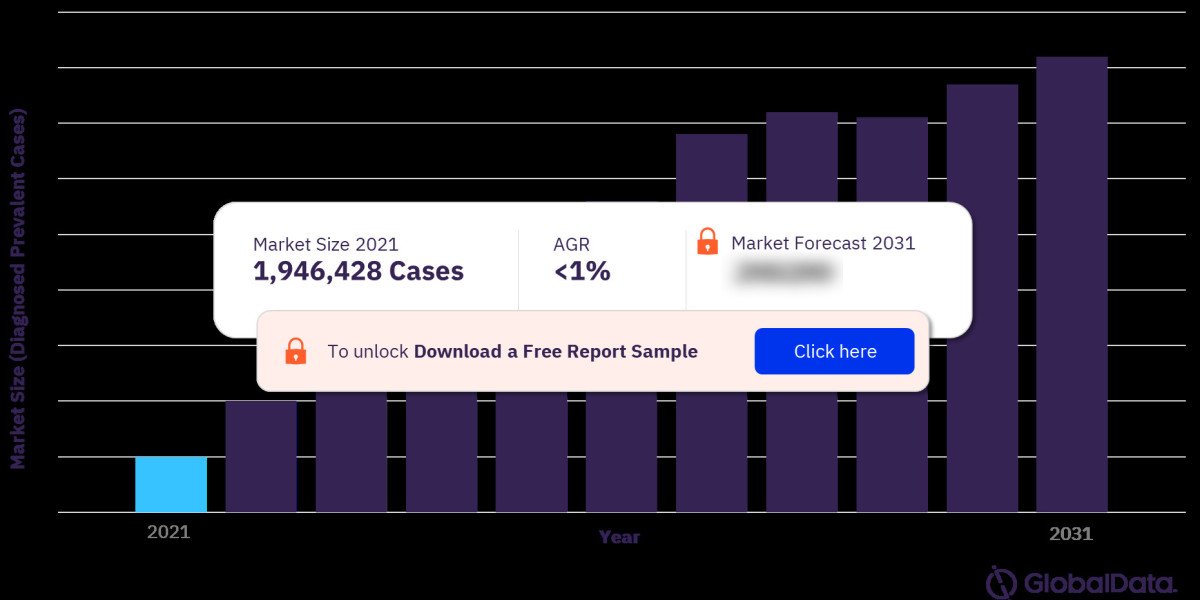
Epidemiology studies the distribution and determinants of health-related states, like UC, in populations. For UC, this includes tracking prevalence (existing cases) and incidence (new cases) worldwide. For more insights into the Ulcerative Colitis market forecast, download a free report sample
Regional Trends in Ulcerative Colitis Prevalence
- North America and Europe: UC prevalence is highest in these regions, with estimates ranging from 120 to 250 cases per 100,000 individuals.
- Asia and Africa: Traditionally low prevalence, but incidence rates are rising due to urbanization and lifestyle changes.
- Oceania and Latin America: Emerging regions for UC research, reflecting intermediate prevalence levels.
Age and Gender Disparities
- UC is often diagnosed between 15–30 years of age, with a smaller peak in incidence at 50–70 years.
- The disease affects men and women equally, though slight gender differences may exist in specific populations.
Risk Factors Associated with Ulcerative Colitis
Genetic Predisposition
Family history of IBD significantly increases the risk of developing UC, with several genes identified as contributors to susceptibility.
Environmental Triggers
- Dietary Patterns: Diets high in fats and processed foods may increase risk, while fiber-rich diets might offer protective effects.
- Urbanization: Increased exposure to industrial pollutants and reduced microbial diversity are linked to higher UC prevalence.
Lifestyle Factors
- Smoking: Unlike Crohn’s disease, UC prevalence is higher among non-smokers or those who quit smoking.
- Stress: Chronic stress can exacerbate symptoms and potentially increase disease risk.
Microbiome Alterations
Imbalances in gut microbiota are strongly associated with UC, contributing to immune dysregulation and inflammation.
Comorbidities and Complications
Comorbid Conditions
Patients with UC often face additional health challenges, such as:
- Arthritis (enteropathic arthritis)
- Primary sclerosing cholangitis (PSC)
- Osteoporosis
- Mental health disorders, including anxiety and depression
Long-Term Complications
- Colorectal Cancer (CRC): Prolonged inflammation increases the risk of CRC, necessitating regular screenings.
- Severe Flares: Acute episodes can lead to complications like toxic megacolon or perforation.
Epidemiological Trends and Emerging Concerns
Rising Incidence in Emerging Economies
The increasing prevalence of UC in Asia, Africa, and Latin America reflects rapid urbanization, changing diets, and improved diagnostic capabilities.
Impact of Globalization
Migration patterns reveal that individuals from low-risk regions adopting Western lifestyles exhibit increased UC risk.
Influence of the COVID-19 Pandemic
Disruptions in healthcare access and stress during the pandemic impacted UC diagnosis and management, necessitating further epidemiological studies.
Current Research and Data Gaps
Geographical Variability
While extensive data exists for North America and Europe, there’s a lack of comprehensive research from low- and middle-income countries.
Pediatric UC
Limited studies focus on childhood-onset UC, though it presents unique clinical challenges and long-term implications.
Microbiome-Immune Interactions
Exploring the role of gut microbiota in UC pathogenesis remains a key area for future research.
Preventive Strategies and Management
Raising Awareness
Public health campaigns emphasizing lifestyle modifications can help mitigate risk factors associated with UC.
Dietary Interventions
Promoting balanced, anti-inflammatory diets may reduce disease risk and improve outcomes in affected individuals.
Early Screening and Diagnosis
Improved access to diagnostic tools, such as colonoscopy and biomarkers, enables early detection and intervention.
FAQs
What is the global prevalence of ulcerative colitis?
The global prevalence varies, with the highest rates in North America and Europe (120–250 cases per 100,000) and rising incidence in Asia and Africa.
What are the primary risk factors for ulcerative colitis?
Genetic predisposition, environmental factors, dietary habits, lifestyle changes, and gut microbiota imbalances contribute to UC risk.
Why is UC incidence rising in emerging economies?
Urbanization, dietary shifts, and increased healthcare access for diagnostics are driving higher incidence rates in these regions.
How does UC differ between pediatric and adult populations?
Pediatric UC often presents with more extensive disease and may have different long-term implications compared to adult-onset UC.
Can UC lead to colorectal cancer?
Yes, chronic inflammation from UC increases the risk of colorectal cancer, especially in long-standing or severe cases.
What role does the microbiome play in UC?
Gut microbiota imbalances contribute to immune dysregulation and inflammation, playing a critical role in UC pathogenesis.
Conclusion
The Ulcerative Colitis Epidemiology Analysis underscores the growing burden of UC worldwide. With rising prevalence and evolving risk factors, understanding the epidemiological trends of this condition is vital for developing effective prevention and management strategies. By addressing research gaps, improving diagnostics, and fostering global collaboration, the healthcare community can enhance outcomes for individuals living with UC.